Case report - Individualized Single Tooth
Dr. med. dent. Sebastian Horvath
Curriculum vitae
Dr. Sebastian Horvath specializes in esthetic-restorative treatments, as they combine many aspects of modern dentistry and have a positive impact on his patients. He works together with his wife and father in the group practice Dr. Horvath in Jestetten, Germany. Dr. Horvath is a native of Jestetten and studied dentistry at the University of Freiburg, Germany, from 2003-2008. In 2008, he received his doctorate (Dr. med. dent.) from the same university. From 2009-2012, he worked as a research assistant at the Department of Prosthodontics at the University Hospital of Freiburg, Germany, and completed training as a qualified advanced specialist in prosthodontics. As part of the specialization, he received in-depth training in fixed prosthodontics, esthetic dentistry, implantology, and all-ceramic materials. In 2012 he was awarded the "Young Esthetics Award" of the German Society for Esthetic Dentistry (DGÄZ).
Introduction
Growing health concerns of patients have led to an increas-ing demand of metal-free restorations. The same is true for dental implants. As dental professionals it is our goal to ful-fil this demand of our patients in the most predictable way. When it comes to implant treatments the two most cru-cial aspects regarding a treatment success are the osse-ointegration of the implant and the prosthetic workflow. The Patent™ implant system features a novel zirconia implant design with an innovative prosthetic connection. In a pro-spective cohort study by Becker et al. 2017, the Patent™ implant system was evaluated for posterior single tooth ap-plications with good results. The survival rate was 95.8 % after two years. A very positive soft tissue response was also reported. This is in line with what was reported by Brüll et al. 2014, in a 3-year retrospective follow-up. The follow-ing case report shows the replacement of a lower molar using the Patent™ zirconia implant system.

Dr. med. dent. Sebastian Horvath
Bahnhofstrasse 24
79798 Jestetten, Deutschland
https://www.drhorvath.de/
Telephone +49 7745 7211 kontakt@drhorvath.d
Initial Situation
A 54-year old female patient presented at the author’s office, asking for a general restoration of her teeth. As a part of this complex case the lower right quadrant was restored (Figs. 1 & 2). The treatment of this area is the subject of this case report. The patient reported that the old restoration was placed about 20 years ago after tooth #46 was lost due to endodontic complications. A few years after the placement of the restoration tooth #45 was endodontically treated through the placed res-toration. Now the patient reported an increasing sensitiv-ity on tooth #47 due to ill-fitting margins. It was planned to restore the area with two all-ceramic crowns on teeth #45 & 47, and an implant-retained restoration in site #46. The implant-retained restoration was preferred to a new fixed dental prosthesis in order to reduce the load on the endodontically treated tooth #45 and to reduce future risks by incorporating an endodontically treated tooth in a larger restoration. Initially, a CBCT was made in order to evaluate the bone volume in the edentulous areas and to evaluate existing root canal treatments.
Pretreatment
The CBCT revealed sufficient bone volume in site #46 to place an implant (Fig. 3). A custom implant was designed in order to get the optimal transgingival design for this individual case. The intrabony part of the implant had the di-mensions 4.5 x 9 mm. The old fixed dental prosthesis was removed and tooth #45 built-up with a post and core res-toration. Subsequently, a digitally planned provisional res-toration was fabricated and placed. The scan for the pro-visional restoration was further used for the fabrication of a surgical guide. For this, the scan was matched to the CBCT on the contralateral posterior teeth and the anterior teeth as they remained unchanged from the initial situation.

Fig. 1:
Initial situation in the lower right quadrant. The patient reported about increasing sensitivity on tooth #47.

Fig. 2:
Initial radiograph showing the lower right quadrant. Note the ill-fitting margin distal on tooth #47.
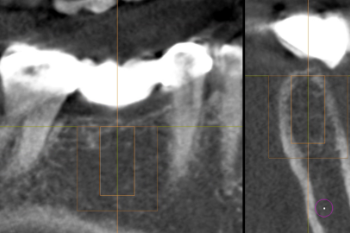
Fig. 3:
A CBCT revealed sufficient bone volume in site #46 to place an implant.
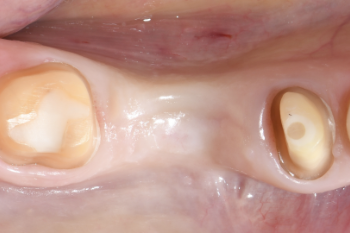
Fig. 4:
Clinical situation prior to the surgery.
Implant Placement
The fit of the surgical guide was evaluated prior to the surgery (Fig. 5). Following local anaesthesia, a full-flap in site #46 was elevated to gain access to the bone (Fig. 6). The incision was performed centrally on the ridge in order to evenly space out the attached gingiva on the lingual and buccal sides. Subsequently, a guided osteotomy was performed according to the manufacturers recommen-dations (Fig. 7). The drilling protocol for hard bone was used, which includes a cortical drill and a screw tap. The implant was placed and a sufficient primary stability of 30 Ncm was achieved (Fig. 8). The insertion torque was measured electronically during the placement of the im-plant. The incision was closed and the prosthetic connec-tion sealed using Teflon tape (Figs. 9–11). A new, digitally planned provisional restoration was fabricated (Fig. 12). In the area of the newly placed implant the provisional res-toration was planned as a flat pontic towards the implant with a distance of about .1 mm between the implant and the provisional restoration. This design facilitated good cleaning in the following weeks and also ensured that the implant was unloaded during healing. Sutures were re-moved ten days postsurgery. Healing was uneventful.
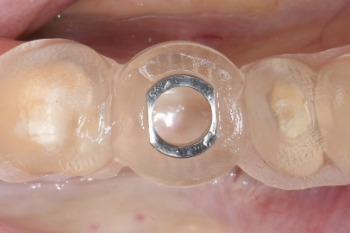
Fig. 5:
The placed surgical guide.
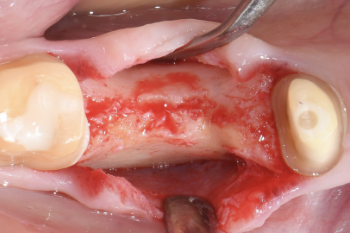
Fig. 6:
A full-flap was elevated to gain access to the bone.
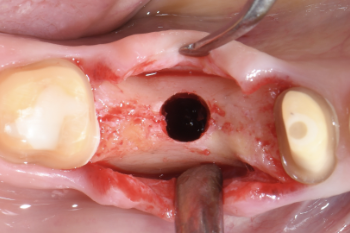
Fig. 7:
The osteotomy was performed using the drilling protocol for hard bone.
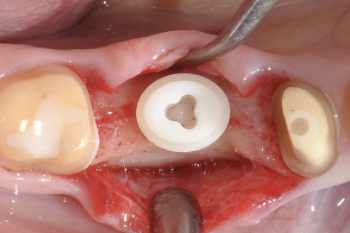
Fig. 8:
The custom-planned zirconia implant was placed and a sufficient primary stability of 30 Ncm achieved.

Fig. 9:
Wound closure.

Fig. 10:
The prosthetic connection was sealed using Teflon tape.
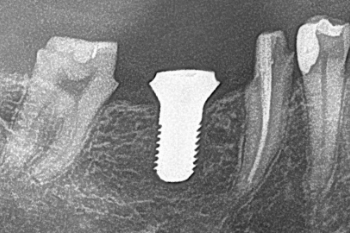
Fig. 11:
Radiographic evaluation of the implant position.

Fig. 12:
In the area of the newly placed implant the provisional restoration was planned as a flat pontic towards the implant with a distance of about .1 mm between the implant and the provisional restoration.
Prosthetic Reconstruction

Fig. 13:
Clinical situation three months after implant placement. Healing was uneventful.

Fig. 14:
The implant was stable and the soft tissue presented itself as healthy.

Fig. 15:
Occlusal view.

Fig. 16:
For the prosthetic reconstruction a glass fibre post and core assembly was adhesively cemented on the implant.

Fig. 17:
The post and core assembly is pre-fabricated and tightly fits into the implant connection.

Fig. 18:
Following this build-up, the implant was prepared for a full-crown restoration just like a natural tooth.

Fig. 19:
Occlusal view.
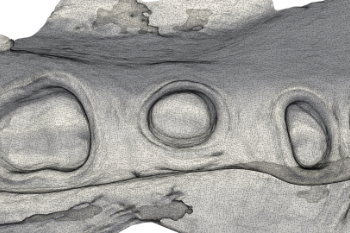
Fig. 20:
An intra-oral scan was performed for a lab-side prosthetic workflow.
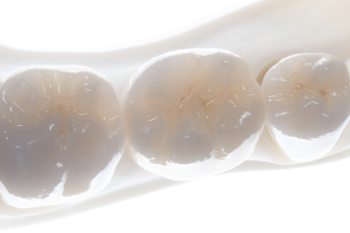
Fig. 21:
Three monolithic zirconia crowns were fabricated (Ceramics: MDT Claus-Peter Schulz).

Fig. 22:
Intra-oral view of the treatment result.

Fig. 23:
Occlusal view.

Fig. 24:
Radiographic evaluation of the treatment result.

Fig. 25:
Situation at the 1-year follow-up.





