About the author
Vienna-based specialist Dr. Harald Fahrenholz has been practising dental implant surgery for more than thirty years. He has been working in and leading several different dental practices over the past three decades. Today, Dr. Fahrenholz is lecturing on implant treatment and implant prosthetics at dental conferences worldwide, in addition to his daily clinical work in his own practice “Zahnästhetik am Kohlmarkt” in the first municipal district of Vienna, in which he follows a strict biological approach.
Contact
Zahnästhetik am Kohlmarkt
Kohlmarkt 7/1/4/34
1010 Vienna, Austria
+43 1 8905947
Today, practitioners have to meet growing patient demand for esthetic tooth replacements that remain healthy in the long term, often involving immediate implant placement and loading. In the following article, a case is presented in which the patient’s esthetic zone was restored using a two-piece zirconia implant system which has been an integral part of the author’s clinical armamentarium for more than ten years. In clinical studies, this implant system has demonstrated healthy and stable hard- and soft-tissue conditions as well as excellent esthetics.[1, 2] It is therefore ideally suited for the indication described.
Initial situation
The 41-year-old female patient presented to the author’s practice in October 2021. Owing to a failing post and core restoration of an endodontically treated tooth #11, she expressed the desire for a metal-free implant-supported restoration in this area (Figs. 1 & 2). The radiographic evaluation by means of CBCT revealed that there was sufficient bone volume in the site for the planned implant placement (Fig. 3).

Figure 1
Frontal view of the initial situation.

Figure 2
Occlusal view of the initial situation.

Figure 3
Radiographic view of the initial situation.
Treatment planning
As part of the surgical procedure, it was planned to remove the failing restoration, extract the remaining tooth root and immediately insert a two-piece zirconia implant (Patent™ Dental Implant System, Zircon Medical Management) into the extraction socket. Furthermore, it was planned to prepare the glass fiber post and core assembly, which serves as the prosthetic buildup of the implant system used, chairside in the same treatment session, to adhesively cement it on to the implant and to restore it with a provisional crown so that the patient could leave the dental practice after surgery without a missing tooth.
Surgical procedure
After local anesthesia had been administered, a labial incision was made in the region of tooth #11 to facilitate the removal of the failing tooth (Fig. 4). After the old restoration had been removed (Fig. 5), the underlying tooth root was extracted (Figs. 6 & 7), and the extraction socket was carefully curetted to completely remove any fibrous tissue (Fig. 8). The osteotomy was prepared according to the drilling protocol of the implant manufacturer and under water cooling (Fig. 9). Once prepared, the osteotomy was treated with ozone to disinfect and sterilize the implant bed (Fig. 10). Thereafter, the two-piece zirconia implant with a diameter of 4.5 mm and a length of 13.0 mm was removed from the implant sleeve using an insertion tool (Fig. 11) and inserted into the osteotomy (Fig. 12). The implant was screwed into the bone using the torque wrench provided by the implant manufacturer (Fig. 13), up to a maximum torque of 35 N cm. High primary stability of the inserted implant was achieved (Fig. 14).

Figure 4
Labial incision for removal of the failing tooth.

Figure 5
Remaining root #11 after removal of the old crown.

Figure 6
Root extraction.

Figure 7
Root extraction.

Figure 8
Thorough curettage of the extraction socket.

Figure 9
Osteotomy preparation according to the drilling protocol of the manufacturer.
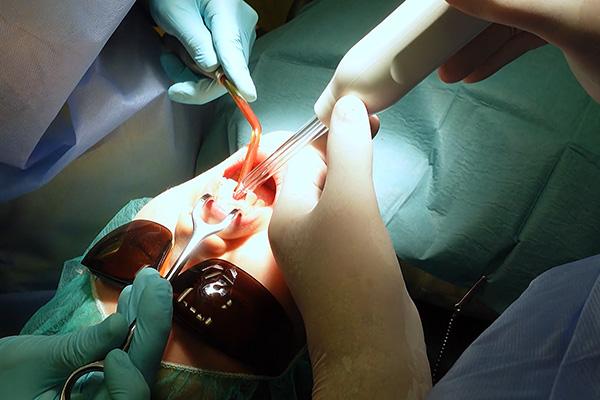
Figure 10
Ozone therapy of the implant bed.

Figure 11
Removal of the implant from the sleeve using the insertion tool.

Figure 12
Insertion of the implant into the osteotomy.

Figure 13
Insertion of the implant using the torque wrench of the manufacturer.

Figure 14
Inserted implant after achieving high primary stability.
Prosthetic restoration and healing
Immediately after implant insertion, the prefabricated glass fiber post was prepared extraorally using a diamond bur and fitted into the 3C platform of the placed implant for try-in. The final preparation of the post was carried out intraorally (Fig. 15). After try-in of the provisional crown, which was fitted on to the prepared glass fiber post, both the post and provisional crown were removed again. The 3C platform of the implant was filled with a dual-polymerizing cement (RelyX Unicem 2, 3M ESPE), and the prepared glass fiber post was inserted into it (Fig. 16). Excess cement was removed and the glass fiber post was light-polymerized (Fig. 17). The glass fiber post was isolated with Vaseline oil, and the provisional crown was subsequently cemented using a temporary cement mixture (Figs. 18–20). One week after surgery, the patient presented to the author’s dental office for a follow-up appointment. Already at this time, an extremely beneficial and healthy soft-tissue reaction around the neck of the inserted implant was evident. After successful osseointegration and an uneventful healing period of three months, the definitive crown was delivered (Figs. 21 & 22). At the 12-month follow-up, the soft-tissue conditions were considered healthy and stable, and the treatment result was deemed satisfactory from an esthetic point of view (Fig. 23).

Figure 15
Intraoral preparation of the glass fiber post after try-in.

Figure 16
Light polymerization of the cement.

Figure 17
Cemented prepared post.

Figure 18
Cementation of the provisional crown on to the prepared glass fiber post.

Figure 19
Frontal view of the clinical situation after delivery of the provisional restoration.

Figure 20
Occlusal view of the clinical situation after delivery of the provisional restoration.

Figure 21
Frontal view of the clinical situation after delivery of the definitive restoration after three months of healing.
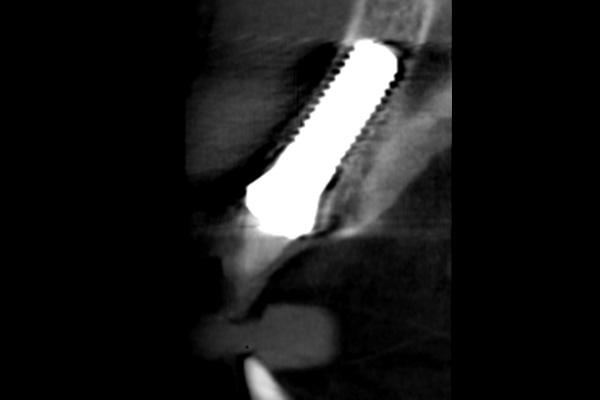
Figure 22
Radiograph of the final result after three months of healing.

Figure 23
Frontal clinical view of the final result after 12 months.
Discussion
The two-piece zirconia implant system used for the clinical case described is routinely and almost exclusively used in the author’s practice. Thanks to its very rough endosteal surface, reliable bone healing is to be expected.[3] One of the main challenges in cases of immediate implant placement in the anterior region, like that described here, is the preservation of the alveolar bone (and the buccal plate in particular) during extraction. Also, correct positioning of the planned implant and the direction of insertion are of great importance to prevent the implant from penetrating the buccal bone. For this reason, it is necessary to drill slightly more palatally from the alveolar direction. Also, having a tissue-level design, the implant used is placed at the equigingival level, which means that its crown margin is clearly visible and accessible during the entirety of the prosthetic procedure. For the same reason, excess cement can be easily and completely removed after cementation of the glass fiber post. As a result, the risk of cementitis due to subgingival cement remnants is virtually nonexistent. Moreover, as a result of implant positioning equigingivally, and to the proper depth, too high a compression on the cortical bone is avoided, which would otherwise adversely impact marginal bone stability.[4] Furthermore, the glass fiber post used for the core buildup of the two-piece implant system used, offers added value regarding stability: Having a dentinlike modulus of elasticity, the glass fiber post attenuates masticatory forces transferred from the superstructure to the implant, minimizing the fracture risk of the implant components as a result. Post preparation by means of a diamond bur is done in the same way a natural tooth or a post and core in endodontic dentistry would be prepared.
Conclusion
With the two-piece zirconia implant system used in the clinical case described, esthetic restorations in the anterior area can be realized thanks to its natural-looking shade and its beneficial soft-tissue integration. Also, thanks to its tissue-level design, which avoids a microgap at the subgingival level, and the tissue-friendly and plaque-resistant implant material, zirconia, long-term successful treatment outcomes with minimal risk of biological late-term complications like periimplantitis can be expected. The author has not experienced a single case of periimplantitis in the more than ten years for which he has been using this implant system.
References:
1 Brüll F, van Winkelhoff AJ, Cune MS. Zirconia dental implants: a clinical, radiographic, and microbiologic evaluation up to 3 years. Int J Oral Maxillofac Implants. 2014 Jul-Aug;29(4):914-20. doi: 10.11607/jomi.3293. PMID: 25032772.
2 Becker J, John G, Becker K, Mainusch S, Diedrichs G, Schwarz F. Clinical performance of two-piece zirconia implants in the posterior mandible and maxilla: a prospective cohort study over 2 years. Clin Oral Implants Res. 2017 Jan;28(1):29-35. doi: 10.1111/clr.12610. Epub 2015 May 6. PMID: 25951536.
3 Glauser, R., Schupbach, P. Early bone formation around immediately placed two-piece tissue-level zirconia implants with a modified surface: an experimental study in the miniature pig mandible. Int J Implant Dent 8, 37 (2022). https://doi.org/10.1186/s40729-022-00437-z
4 Fiorillo L, Milone D, D’Andrea D, Santonocito D, Risitano G, Cervino G, Cicciù M. Finite Element Analysis of Zirconia Dental Implant. Prosthesis. 2022; 4(3):490-499. https://doi.org/10.3390/prosthesis4030040






