
About the author
Dr. Roland Glauser graduated from the University of Zurich, where he also became Assistant Professor at the Department for Fixed Prosthodontics and Dental Materials. He is an active member of the AO and the EAO, among others. In his research he focuses on tissue integration of dental implants and shortened clinical protocols. Dr. Glauser leads a private clinic in Zurich. He has published an animal model study together with Dr. Peter Schüpbach, in which he found that Patent™ Implants reach a BIC value of over 70% after only four weeks of healing.Contact
Cosmodent–Zahnärzte am Bahnhofsplatz
Bahnhofplatz 9
8001 Zurich, Switzerland
+41 44 266 1111
Introduction
Recent years have seen a continuous increase in the demand for zirconia dental implants as a result of growing public health awareness and a surge in material sensitivity cases. For one thing, zirconia implants elicit little inflammatory reaction from the peri-implant tissue and provide a particularly high degree of epithelial attachment. In addition, zirconia implants have a rather natural appearance owing to their white, almost tooth-like color, facilitating highly esthetic treatment outcomes. For these reasons, among others, zirconia implants pose a viable treatment option for restoration of missing teeth or the replacement of failing restorations in the anterior region. However, implant placement in the esthetic zone can pose significant clinical challenges. In cases with atrophic changes to the alveolar crest or limited space (especially in the anterior mandible), narrow-diameter implants might be indicated. In the following, Zurich-based dental implant specialist and researcher Dr Roland Glauser presents a clinical case in which a failing post and core restoration in the anterior mandible had to be removed and restored using a narrow-diameter zirconia implant and a crown. The manufacturer of the implant system used offers the possibility of designing dental implants individually using proprietary software, allowing Dr Glauser to tailor the planned implant to the anatomical conditions of the patient.
Initial situation
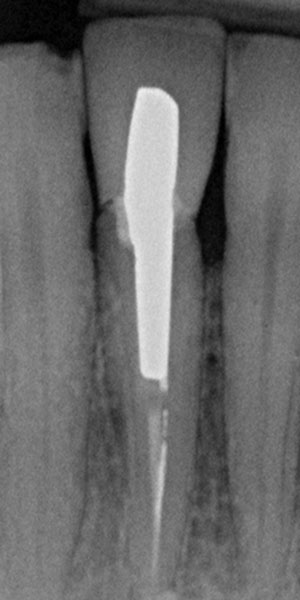
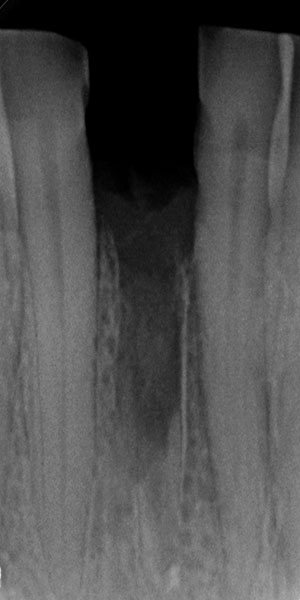
The 45-year-old male patient was referred to my practice. He presented for initial consultation complaining about a crown on his endodontically treated tooth #41 that had become loose. The patient had an accident in his youth which resulted in the traumatic facture of the mandibular right central incisor. As a result, the tooth had to be endodontically treated and was restored with a gold post and core and a veneered ceramic crown (Fig. 1). The crown had been in situ without complications for 22 years. Upon removing the failing crown and the post, a vertical root fracture was discovered (Fig. 2). Therefore, the remaining root was deemed unsalvageable.



Treatment planning
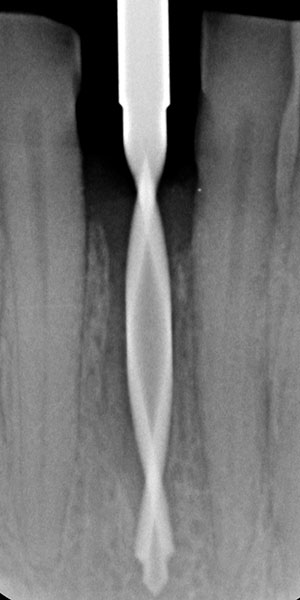
Treatment would involve the extraction of root #41, and the restoration of this area with an immediate implant with immediate function using a provisional crown. Before the surgery, the dental laboratory conducted a spatial analysis on a study model. Additionally, the tooth to be extracted was ground off the stone model, and an implant analogue was placed in the ideal position. Thereafter, the glass fiber post was prepared on the model, and a shell provisional prosthesis was fabricated (Fig. 3). It incorporated wings to be placed on the neighboring teeth to allow its correct positioning.

Surgical procedure
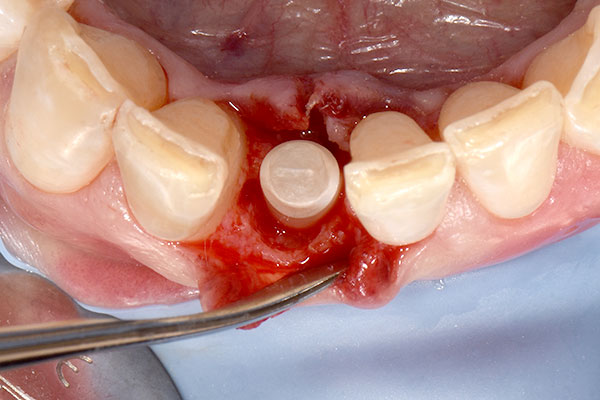
After local anesthesia had been administered, a rubber dam was placed for isolation and optimum control of the operative site. Root #41 was then extracted, and the extraction socket was carefully curetted to remove any fibrous tissue and examined (Fig. 4). The osteotomy for the immediate implant was prepared according to the drilling protocol of the implant manufacturer (Fig. 5). An individual two-piece narrow-diameter zirconia implant of 3.5 mm in diameter and 13.0 mm in length (Patent™ Dental Implant System, Zircon Medical Management), which was designed ahead of surgery, was inserted into the prepared osteotomy to a final torque of 28 N cm, achieving adequate primary stability to proceed with the provisional prosthesis and immediate function (Fig. 6).




Provisional prosthesis and soft-tissue augmentation
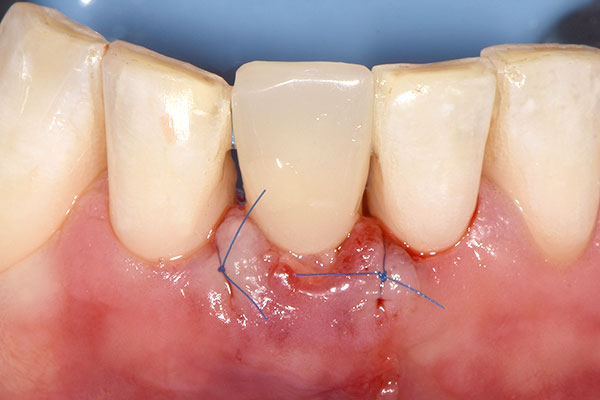
Immediately after implant placement, the glass fiber post, which was prepared in advance by the dental laboratory, was inserted into the 3C connection of the implant and cemented in place using RelyX™ Unicem dental cement (3M™; Fig. 7). Afterwards, a guided bone regeneration procedure was performed using Bio-Oss Collagen® and a resorbable Bio-Gide® membrane (Geistlich Pharma) to fill the gap between the wall of the extraction socket and the implant (Figs. 8 & 9). A circular hole was punched in the membrane to allow it to be placed over the grafted site with the implant penetrating through, enabling provisionalization. The post was then isolated with Vaseline oil to facilitate the finishing of the shell provisional prosthesis. The provisional prosthesis was relined on the post with flowable composite (Fig. 10). The wings were subsequently cut off, and the crown was polished. The crown was cemented using a temporary cement (Temp-Bond™, Kerr Dental), and a lingual vent hole allowed for excess cement to be evacuated. A connective tissue graft was placed labially to bulk up the soft tissue and increase volume (Fig. 11). The grafted site was finally sutured closed (Fig. 12).






Healing and definitive restoration
At the three-week follow-up, healing was considered uneventful (Fig. 13). At the nine-month follow-up (Fig. 14), a conventional full-arch impression was taken, which served as the basis for the fabrication of the master model and the definitive crown by the dental laboratory (Figs. 15 & 16). At the ten-month follow-up, the definitive prosthesis was delivered (Fig. 17). At the 12-month follow-up, the definitive prosthesis was considered highly esthetic, and the peri-implant soft-tissue conditions were stable and healthy (Fig. 18).








Discussion
Restoring mandibular incisors with dental implants is a surgical and prosthetic challenge owing to the lack of space. Treatment planning with the final prosthetic outcome in mind is critical. The procedure described here employs a guided approach based on the crown position. Surgically, immediate placement requires a more lingual position of the implant, leaving some space between the implant and buccal plate, hence the guided bone regeneration procedure, in which some bone substitute was placed in the gap to support the buccal plate and maintain volume. To further enhance esthetics and volume, a fibrous tissue graft was placed just under the cervical part of the crown. Moreover, the implant used incorporates a true soft-tissue-level design and is placed at the equigingival level. This means that its crown margin is clearly visible and accessible during the entirety of the prosthetic procedure. For the same reason, excess cement can be easily and completely removed after cementation of the glass fiber post. Designing the provisional prosthesis with a vent hole allows any excess cement to be evacuated lingually instead of being pushed down into the sulcus. As a result, the risk of cementitis due to subgingival cement remnants is virtually non-existent.
Conclusion
For implant-supported restorations in the esthetic zone, especially in the anterior mandible, where there might be limited space, the narrow-diameter zirconia implant used in the case described presents a viable treatment option. One year after surgery, the treatment outcome was considered functional and highly esthetic thanks to the beneficial soft-tissue integration of the implant, and an increase of keratinized gingiva could even be observed. Another factor decisive for the excellent treatment outcome was that I was able to design the implant individually in advance using the proprietary design software of the implant manufacturer and, by doing so, tailor it to the unique anatomical conditions of the patient.





